Post treatment of Blood Irradiation High Voltage Power Supply
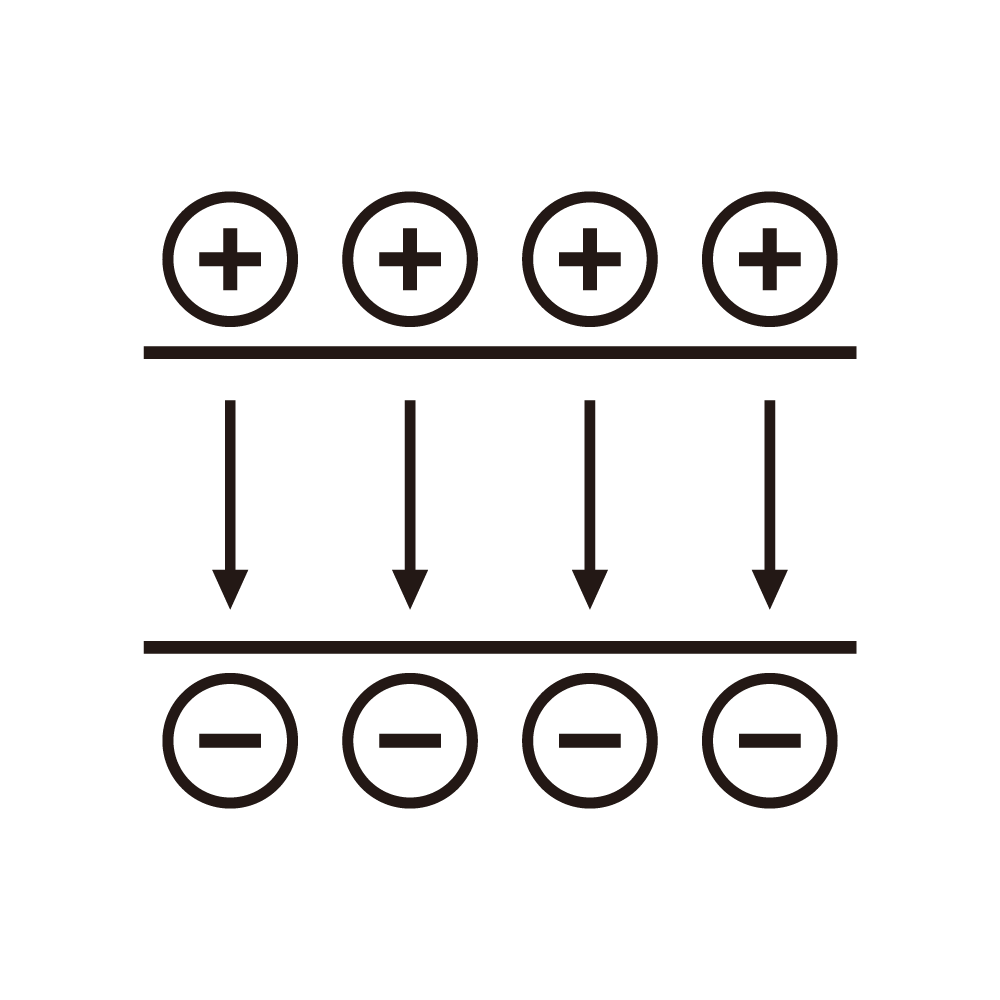
Blood irradiation, as an important means to ensure transfusion safety, uses specific energy rays generated by high voltage power supplies to inactivate lymphocytes in the blood, preventing serious complications such as transfusion associated graft versus host disease (TA GVHD). After the blood irradiation is completed, a proper post treatment process is crucial for ensuring blood quality and the safety of blood recipients.
Firstly, verification of the irradiation dose is a key step in post treatment. Although a specific irradiation dose is preset during the irradiation process by the high voltage power supply, due to the long term use of the equipment, environmental factors, and other influences, there may be deviations in the actual dose. By using a dosimeter, the irradiated blood samples are tested for the dose to ensure that it is within the specified safe dose range. Accurate dose verification not only guarantees the irradiation effect and effectively inactivates lymphocytes but also avoids damage to other effective components in the blood due to excessive dose, maintaining the normal physiological functions of the blood.
Next is a comprehensive test of the quality of the irradiated blood. The functional test of red blood cells is particularly important. It is necessary to evaluate whether their oxygen carrying and oxygen releasing abilities are affected by irradiation. By detecting indicators such as the ATP content and 2,3 diphosphoglycerate (2,3 DPG) level of red blood cells, the changes in their energy metabolism and oxygen affinity can be judged. The activity of platelets is also a key point of detection. Platelets may experience morphological changes and decreased aggregation function after irradiation. Methods such as platelet aggregation tests and flow cytometry can be used to detect the activity and functional integrity of platelets to ensure that they can normally play a role in blood coagulation in the blood recipient. In addition, components such as proteins and coagulation factors in plasma also need to be tested to prevent protein denaturation and inactivation of coagulation factors caused by irradiation, which may affect blood coagulation and transportation functions.
In terms of storage and transportation, irradiated blood needs to be handled strictly in accordance with specified conditions. Blood should be stored in a blood bank refrigerator at a specific temperature. Generally, the storage temperature of red blood cell suspensions is 2 6°C, and the storage temperature of platelets is 20 24°C. The temperature changes in the storage environment should be continuously monitored to prevent adverse effects of temperature fluctuations on blood quality. During transportation, professional blood transport boxes equipped with temperature monitoring equipment and cushioning materials are used to ensure the stability and safety of the blood during transportation and avoid blood deterioration due to factors such as bumps and temperature changes.
It is also essential to record and track the relevant information of irradiated blood in detail. The recorded content includes irradiation time, dose, blood type, test results, and various parameters during storage and transportation. This information not only helps to trace the entire processing process of the blood, discover potential problems in a timely manner but also provides comprehensive data support for subsequent clinical blood transfusions, ensuring the safety and effectiveness of blood transfusion treatment. Only through a rigorous post treatment process for irradiation can the application of blood irradiation high voltage power supplies truly achieve the goal of ensuring transfusion safety and saving patients' lives.