Innovation of High-Voltage Pulsed Power Supplies in Coronary Treatment
1. Introduction
In the field of cardiovascular intervention, the treatment of coronary artery disease is undergoing a revolutionary shift from traditional physical ablation to precise energy intervention. As the core equipment of pulsed electric field (PEF) ablation technology, the performance innovation of high-voltage pulsed power supplies directly affects surgical safety, lesion targeting, and tissue protection. Addressing the thermal damage limitations of traditional radiofrequency ablation, high-voltage pulsed power supplies induce cell apoptosis through non-thermal effects of nanosecond-level pulsed electric fields, providing a new pathway for coronary treatment. This paper explores innovative directions and key technical breakthroughs of high-voltage pulsed power supplies in coronary treatment by integrating biomedical engineering principles and clinical needs.
2. Pulsed Waveform Optimization: From Single Arrays to Dynamic Modulation
Traditional rectangular pulses are prone to electric field attenuation and energy scattering when passing through vascular tissues, leading to insufficient dose in target lesions or damage to surrounding tissues. Innovative strategies must break through waveform design bottlenecks:
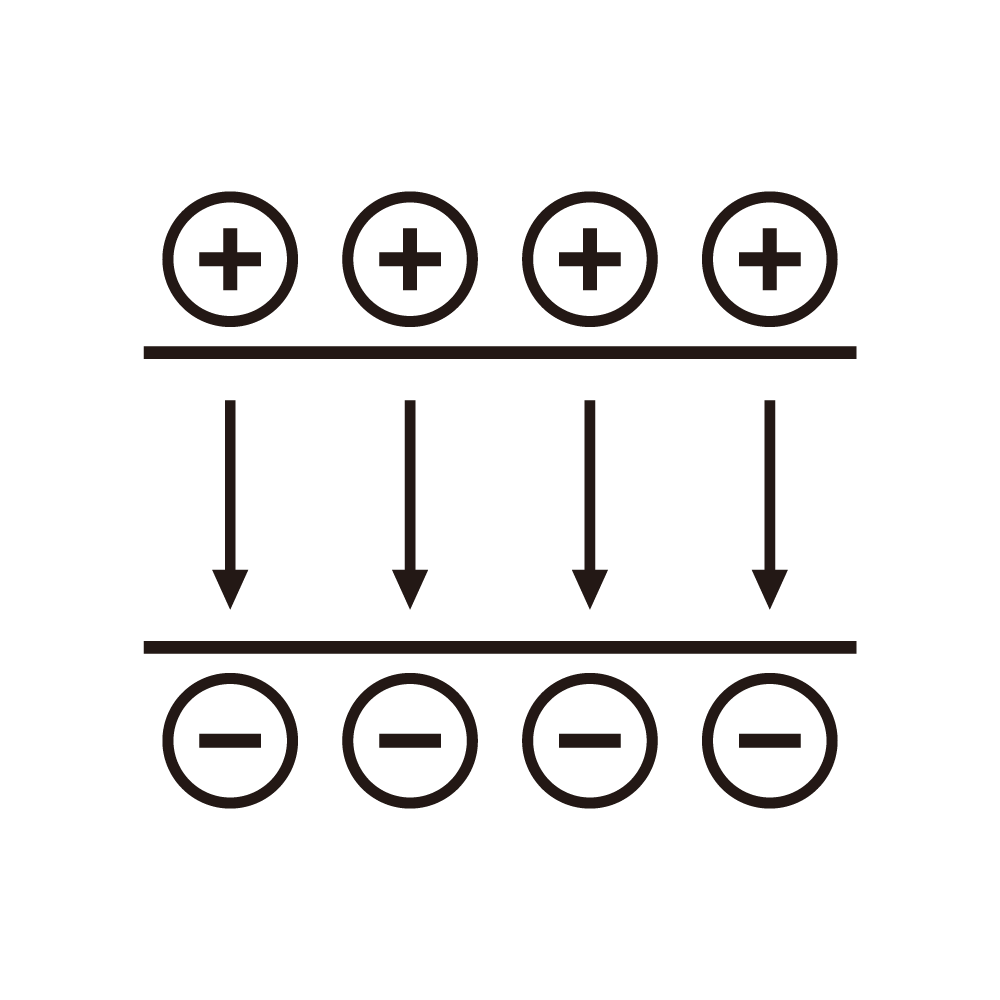
1. Multi-Stage Pulsed Sequence Technology
Develop a cascaded waveform comprising pre-ionization pulses (50-100ns) and main ablation pulses (200-500ns). Pre-ionization pulses enhance cell membrane permeability through instantaneous microporation, increasing main pulse energy utilization by over 30%. Clinical data show that this sequence reduces the ablation threshold voltage from 1.5kV (traditional single pulse) to 1.1kV, significantly lowering the risk of vascular perforation.
2. Adaptive Impedance Matching Regulation
Integrate real-time impedance monitoring modules and reconstruct electric field distribution models based on intravascular ultrasound (IVUS) images. When local impedance mutations caused by plaque calcification are detected, the power supply automatically adjusts the pulse rise edge slope (dynamically adjustable from 10-20kV/μs), focusing energy precisely on fibrotic lesions while reducing normal myocardial cell damage probability to <5%.
3. Precision Control System: From Parameter Presetting to Closed-Loop Feedback
Traditional open-loop control modes struggle to address individual differences in coronary anatomy, making the construction of intelligent closed-loop systems a technical core:
1. Multimodal Sensor Fusion
Integrate intracardiac electrograms (IEGM), optical coherence tomography (OCT), and impedance spectroscopy sensors to establish a multidimensional feature space including apoptosis rate, tissue temperature rise, and membrane potential changes. Through extended Kalman filtering algorithms, sub-millisecond dynamic adjustment of pulse parameters (voltage, frequency, pulse number) is achieved.
2. Intelligent Determination of Treatment Endpoints
Train a support vector machine (SVM)-based tissue damage prediction model. When OCT monitors a cell membrane vesicle formation rate >85% and IEGM shows a local potential amplitude decrease >70%, the system automatically terminates pulse output. This technology reduces average treatment time from 120 seconds (traditional manual control) to 45-60 seconds, minimizing the risk of excessive energy release.
4. Miniaturization and Safety Design: Adapting to Interventional Device Innovation
The minimally invasive trend in coronary intervention imposes strict requirements on the size and safety of high-voltage power supplies:
1. Ultra-Compact Power Unit Integration
Adopt a system-on-chip (SoC) architecture to integrate pulse generators, energy storage capacitors, and control chips, reducing volume to 1/5 of traditional modules (<10cm³). Through multi-layer ceramic capacitor (MLCC) arrays and planar transformer technology, nanosecond-level pulse rise edges and inter-pulse amplitude errors <1% are achieved.
2. Bipolar Insulation Isolation Technology
Design a double-layer electrical isolation structure based on aluminum nitride (AlN) substrates, achieving an insulation strength of 10kVrms between the high-voltage circuit and physiological monitoring circuit. An active discharge protection circuit is introduced to ensure residual voltage decays to safe thresholds within 50μs. In vitro simulation tests show that this design controls leakage risk at the microampere level, meeting IEC 60601-2-77 standards.
5. Clinical Translation Challenges and Future Prospects
Despite the significant advantages of high-voltage pulsed power supplies in coronary treatment, their clinical popularization still faces two major bottlenecks: first, the individual difference mechanisms of pulsed biological effects are not fully understood, requiring the establishment of pre-evaluation models based on genomics; second, long-term efficacy data are insufficient, necessitating multi-center, large-sample randomized controlled trials (RCTs) for validation. Future technological advancements will focus on: ① developing learning-enabled pulsed sequence generation algorithms to achieve personalized lesion-pulse matching; ② exploring synergistic treatment modes with drug-coated balloons to enhance therapeutic efficiency through pulsed drug penetration; ③ integrating magnetic navigation technology to achieve sub-millimeter precise positioning of pulsed electrodes, expanding applications in complex scenarios such as bifurcation lesions.
As a disruptive technology in cardiovascular intervention, the continuous innovation of high-voltage pulsed power supplies will advance coronary treatment toward the ideal goal of precise ablation with zero thermal damage, providing safer and more efficient treatment options for vast numbers of coronary heart disease patients.